South Melbourne 03 9699 2499 | Point Cook 03 8386 7400
Book NowPlantar fasciitis is a painful condition affecting the bottom of the foot. It is a common cause of heel pain and is sometimes called a heel spur. Plantar fasciitis is the correct term to use when there is active inflammation. Plantar fasciosis is more accurate when there is no inflammation but chronic degeneration instead. Acute plantar fasciitis is defined as inflammation of the origin of the plantar fascia and fascial structures around the area. Plantar fasciitis or fasciosis is usually just on one side. In about 30 percent of all cases, both feet are affected.
Anatomy of the Foot
Where is the plantar fascia, and what does it do?
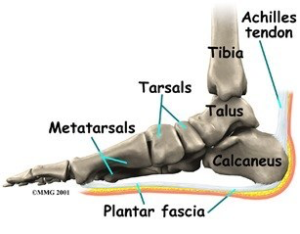
The plantar fascia (also known as the plantar aponeurosis) is a thick band of connective tissue. It runs from the front of the heel bone (calcaneus) to the ball of the foot. This dense strip of tissue helps support the arch of the foot by acting something like the string on an archer’s bow. It is the source of the painful condition plantar fasciitis.
The plantar fascia is made up of collagen fibres oriented in a lengthwise direction from toes to heel (or heel to toes). There are three separate parts: the medial component (closest to the big toe), the central component, and the lateral component (on the little toe side). The central portion is the largest and most prominent.
Both the plantar fascia and the Achilles’ tendon attach to the calcaneus. The connections are separate in the adult foot. Although they function separately, there is an indirect relationship. If the toes are pulled back toward the face, the plantar fascia tightens up. This position is very painful for someone with plantar fasciitis. Force generated in the Achilles’ tendon increases the strain on the plantar fascia. This is called the windlass mechanism. Later, we’ll discuss how this mechanism is used to treat plantar fasciitis with stretching and night splints.

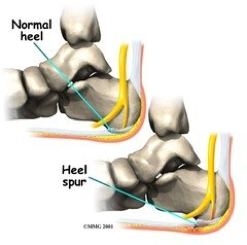
Plantar fasciitis can come from a number of underlying causes. Finding the precise reason for the heel pain is sometimes difficult. As you can imagine, when the foot is on the ground a tremendous amount of force (the full weight of the body) is concentrated on the plantar fascia. This force stretches the plantar fascia as the arch of the foot tries to flatten from the weight of your body. This is just how the string on a bow is stretched by the force of the bow trying to straighten. This leads to stress on the plantar fascia where it attaches to the heel bone. Small tears of the fascia can result. These tears are normally repaired by the body.
As this process of injury and repair repeats itself over and over again, a bone spur (a pointed outgrowth of the bone) sometimes forms as the body tries to firmly attach the fascia to the heel bone. This appears on an X-ray of the foot as a heel spur. Bone spurs occur along with plantar fasciitis but they are not the cause of the problem.
As we age, the very important fat pad that makes up the fleshy portion of the heel becomes thinner and degenerates (starts to break down). This can lead to inadequate padding on the heel. With less of a protective pad on the heel, there is a reduced amount of shock absorption. These are additional factors that might lead to plantar fasciitis.
Some physicians feel that the small nerves that travel under the plantar fascia on their way to the forefoot become irritated and may contribute to the pain. But some studies have been able to show that pain from compression of the nerve is different from plantar fascial pain. In many cases, the actual source of the painful heel may not be defined clearly.
Other factors that may contribute to the development of plantar fasciitis include obesity, trauma, weak plantar flexor muscles, excessive foot pronation (flat foot) or other alignment problems in the foot and/or ankle, and poor footwear.


The diagnosis of plantar fasciitis is generally made during the history and physical examination. There are several conditions that can cause heel pain, and plantar fasciitis must be distinguished from these conditions. Pain can be referred to the heel and foot from other areas of the body such as the low back, hip, knee, and/or ankle. Special tests to challenge these areas are performed to help confirm the problem is truly coming from the plantar fascia.
An X-ray may be ordered to rule out a stress fracture of the heel bone and to see if a bone spur is present that is large enough to cause problems. Other helpful imaging studies include bone scans, MRI, and ultrasound. Ultrasound exam may be favoured as it is quick, less expensive, and does not expose you to radiation.
